Paraovarian cyst
| Paraovarian cyst | |
|---|---|
| Other names | Paratubal cyst, hydatid cyst of Morgagni |
 | |
| Multiple paratubal cysts by a fallopian tube | |
| Specialty | Gynecology |
Paraovarian cysts or paratubal cysts are epithelium-lined fluid-filled cysts in the adnexa adjacent to the fallopian tube and ovary. The terms are used interchangeably,[1] and depend on the location of the cyst.[2]
Pathophysiology
[edit]PTCs originate from the mesothelium and are presumed to be remnants of the Müllerian duct and Wolffian duct.[1]
Diagnosis
[edit]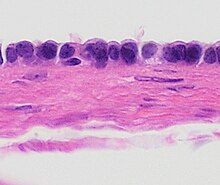
Most cysts are small and asymptomatic.[1] Typical sizes reported are 1 to 8 cm in diameter.[1] PTCs may be found at surgery or during an imaging examination that is performed for another reason. Larger lesions may reach 20 or more cm in diameter and become symptomatic exerting pressure and pain symptoms in the lower abdomen.[3] Large cysts can lead to torsion of the adnexa inflicting acute pain.[3][4]
Prior to surgery, PTCs are usually seen on ultrasonography. However, because of the proximity of the ovary that may display follicle cysts, it may be a challenge to identify a cyst as paratubal or paraovarian.[5]
Malignancy
[edit]PTCs are generally benign, but may, on rare occasions, give rise to borderline tumors and malignancies.[6]
Management
[edit]Smaller lesions can be followed expectantly. Larger lesions, lesions that are growing or symptomatic, and lesions with sonographically suspicious findings (septation, papillations, fluid and solid components) are generally surgically explored and removed.[citation needed]
Epidemiology
[edit]PTCs have been reported in all female age groups and seem to be most common in the third to fifth decades of life.[1][7] A study in Italy estimated their incidence to be about 3%,[1] while an autopsy study of postmenopausal women detected them in about 4% of cases.[8] These cysts constitute about 10% of adnexal masses.[5]
Hydatid cysts of Morgagni
[edit]Hydatid cysts of Morgagni, also hydatids of Morgagni or Morgagni's cysts, are common and appear as pedunculated, often tiny, frequently multiple cysts connected to the fimbriae of the fallopian tubes. They thus appear to be a specific variant of paratubal cysts.[9] They are named after Giovanni Battista Morgagni.
While usually asymptomatic, it has been noted that these cysts tend to be more common in women with unexplained infertility (52.1% versus 25.6% in controls, p<0.001) and suggested that they may play a role in infertility.[10] It has been proposed that these cysts interfere with tubal pick-up and function.[11][12]
References
[edit]- ^ a b c d e f Kiseli M, Caglar GS, Cengiz SD, Karadag D, Yilmaz MB (2012). "Clinical diagnosis and complications of paratubal cysts: Review of the literature and report of uncommon cases". Arch Gynecol Obstet. 285 (6): 1563–69. doi:10.1007/s00404-012-2304-8. PMID 22526447. S2CID 5638006.
- ^ a b Nicole Riddle, Jamie Shutter. "Fallopian tubes & broad ligament, Broad ligament, Paratubal cysts". Pathology Outlines. Topic Completed: 1 July 2013. Minor changes: 30 December 2020
- ^ a b Varras M, Akrivis C, Polyzos D, Frakala S, Samara C (2003). "A voluminous twisted paraovarian cyst in a 74-year-old patient: case report and review of the literature". Clin Exp Obstet Gynecol. 30 (4): 253–6. PMID 14664426.
- ^ Thakore SS, Chun MJ, Fitzpatrick K (2012). "Recurrent ovarian torsion due to paratubal cysts in an adolescent female". J Pediatr Adolesc Gynecol. 25 (4): 85–7. doi:10.1016/j.jpag.2011.10.012. PMID 22840942.
- ^ a b Barloon TJ, Brown BP, Abu-Yousef MM, Warnock NG (1966). "Paraovarian and paratubal cysts: preoperative diagnosis using transabdominal and transvaginal sonography". J Clin Ultrasound. 24 (3): 117–22. doi:10.1002/(SICI)1097-0096(199603)24:3<117::AID-JCU2>3.0.CO;2-K. PMID 8838299. S2CID 20590305.
- ^ Suzuki S, Furukawa H, Kyozuka H, Watanabe T, Takahashi H, Fujimori K (2013). "Two cases of paraovarian tumor of borderline malignancy". Journal of Obstetrics and Gynaecology Research. 39 (1): 437–41. doi:10.1111/j.1447-0756.2012.01953.x. PMID 22889349. S2CID 205512035.
- ^ Damle F, Gomez-Lobo V (2012). "Giant paraovarian cysts in young adolescants: a report of three cases". J Reprod Med. 57 (1–2): 65–7. PMID 22324272.
- ^ Dorum A, Blom GP, Ekerhovd E, Granberg S (2005). "Prevalence and histologic of adnexal cysts in postmenopausal women: an autopsy study". Am J Obstet Gynecol. 192 (1): 48–54. doi:10.1016/j.ajog.2004.07.038. PMID 15672002.
- ^ Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. p. 272. ISBN 9780071716727.
- ^ Rasheed SM, Abdelmonem AM (2011). "Hydatid of Morgagni: a possible underestimated cause of unexplained infertility". Eur J Obstet Gynecol Reprod Biol. 158 (1): 62–6. doi:10.1016/j.ejogrb.2011.04.018. PMID 21620555.
- ^ Abd-el-Maeboud KH (1997). "Hydatid cyst of Morgagni: any impact on fertility?". Journal of Obstetrics and Gynaecology Research. 23 (5): 427–31. doi:10.1111/j.1447-0756.1997.tb00868.x. PMID 9392907. S2CID 33607887.
- ^ Cebesoy FB, Kutlar I, Dikensoy E, Yazicioglu C, Lalayci H (2010). "Morgagni hydatids: a new factor in infertility?". Arch Gynecol Obstet. 281 (6): 1015–7. doi:10.1007/s00404-009-1233-7. PMID 19774388. S2CID 22653583.
